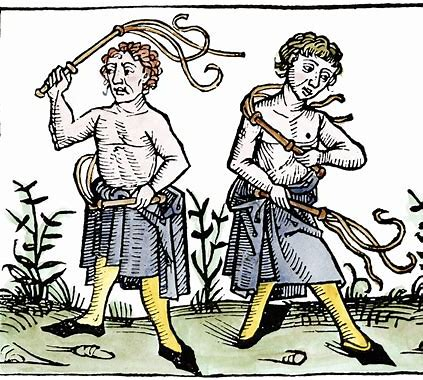
Plan Sponsors Enjoy Pain & Suffering – Embrace Self-Flagellation
The article below (click on link for full article) doesn’t shed light on anything new. These practices have been going on for years. There have been hundreds of lawsuits exposing these egregious practices including Weslaco ISD vs Aetna, Anheiser Busch vs Cigna, Hi-Lex vs Blue Cross, Oakland County vs Blue Cross. Chippewa – Luce- Mackinac Community Action vs BCBS and many more.
It’s all about Working The Spread, that’s where the real money is made.
“Aetna secretly demanded that Optum “bury” its fees into provider claims by tacking on a dummy CPT code and sending Aetna a claim that included both the health care provider’s fee and Optum’s administrative fee. For example, Optum would bill Aetna $70.89 for a claim, of which $34 was its negotiated reimbursement rate and $36.89 was its administrative fee.”
Although practices have been going on for years most plan sponsors have done nothing to protect the interests of plan members. Self-flagellation best describes their behavior.
“This blog highlights several examples of questionable insurer-TPA practices that court cases have uncovered in recent years. Many of these practices may violate ERISA’s fiduciary duties, including requirements that health plan fiduciaries like TPAs act “solely in the interest of the participants and beneficiaries of the plan” when administering a health plan and dispensing its assets. Problematic TPA practices may also—directly or indirectly—contribute to excessive health care spending by health insurance plans and, ultimately, the members and sponsors footing the bills.”
Questionable Conduct: Allegations Against Insurers Acting as Third-Party Administrators | CHIRblog

