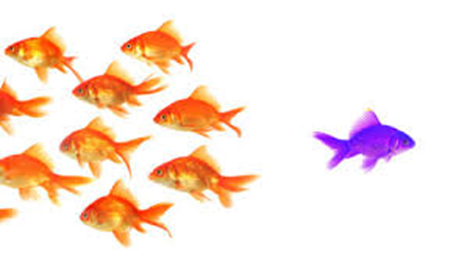
Legacy TPA’s are slow to adapt to market changes and even slower investing in the latest technology whereas new, “upstart” TPA’s invest in the latest technology giving them a distinct advantage.
SOURCE: Yuzu Health | Automating Health Plan Administration
Healthcare in the US is deeply fractured. Between when someone sees a doctor and when insurance pays the bill, there is a dizzying amount of negotiating and coordination that has resulted in an opaque and extremely rigid system reliant on vendors on top of vendors.
We’re on a mission to simplify health plan administration from the ground up, starting with claims processing as a third-party administrator. We believe not only that AI can streamline manual processes but that it will also enable more innovative plan designs to come to market with different covered services and incentive structures. Healthcare needs new ideas in how to deliver care, and we’re building the foundations to enable just that.
What are you exactly?
We’re a third-party administrator that also provides clients with a suite of software tools that improve the experience for the plan manager and the member.
What states are you licensed in?
We are fully licensed to adjudicate claims in the majority of U.S. states, with plans to become licensed nationwide. Please reach out to us for details!
What plan designs do you support?
We support traditional network-based plans as well as newer models like reference based pricing, direct primary care, and cash pay.
With how we built out our technology, our edge is our ability to support atypical plan designs that others can’t support. If you have a new, unique health plan, please reach out!
What vendors do you use and can you support mine?
We’ve consolidated a lot of the tooling TPAs generally outsource, enabling us to integrate with provider networks, PBMs, etc. quite literally on a phone call rather than the usuals weeks of back and forth.

