“As more and more of these cases make their way through the courts, self-insured health plan administrators charged with properly monitoring and safeguarding plan assets should do so, independent of their TPA’s own reporting.”
Federal Judge’s Decision Creates Possible Windfall for Self-Insured Employer Plans; Certifies Class in Case Against Aetna/Optum;
By Mark Flores
June 6, 2023
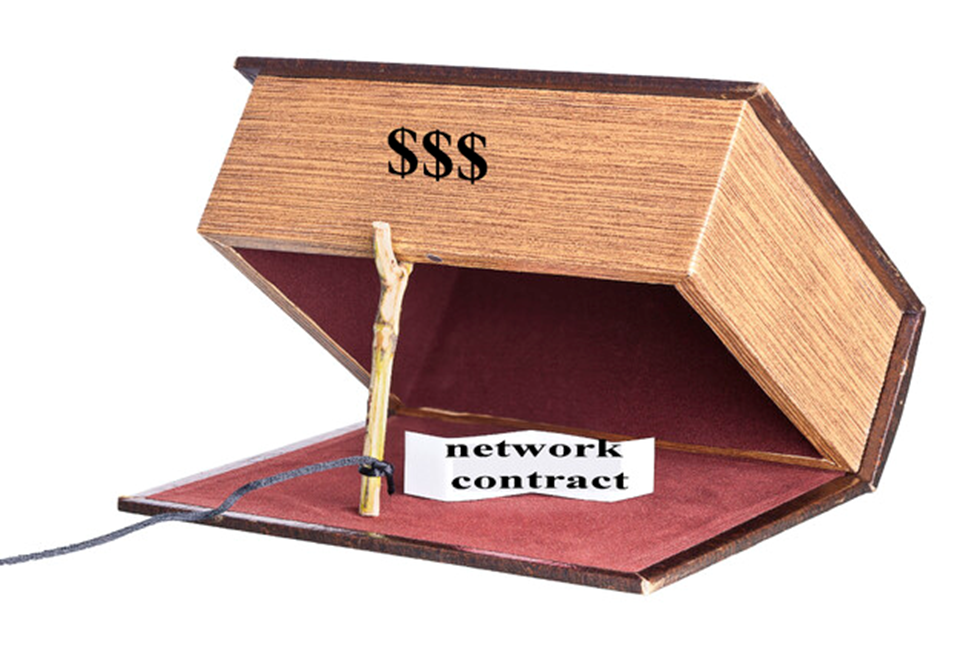
On June 5, 2023, a federal judge granted class certification in a case alleging Aetna & Optum colluded to charge employer plans and participants “Hidden Fees” by inflating medical provider claims using “dummy codes”. All self-insured employer plans are advised to review their own claims experience to ensure they are not being charged “Hidden Fees” by disguising them as Medical Service fees.
As we have written about before, this monumental decision raises alarm bells for all Self-insured group health plans, particularly those that give their TPA or carrier, such as Aetna, authority to pay claims benefits on their behalf.
The alleged outrageous behavior by Aetna and Optum raise questions as to whether all their self-insured plan clients unknowingly overpaid for certain claims and thus be entitled to significant recovery of Plan Assets.
The case revolves around a member of a Self-insured employer plan, Mars Co. where the Plan hired Aetna to assist with Claims Administration duties, which included processing the member’s claims for the Plan and providing a cost-effective network of health care providers. Aetna subsequently subcontracted with Optum to provide chiropractic and physical therapy services to Plan members for more cost-effective prices than Aetna could get on its own.
Rather than pay Optum out of the fees Aetna received from the Self-insujred employer plan, Aetna and Optum agreed to “bury” Optum’s fee within the claims submitted by Optum’s providers via a “dummy code” from the CPT code to reflect a bundled rate fee that would be paid by the participants and the Plan based on their annual out-of-pocket maximums.
In other words, the Plan and the members paid for Optum’s administrative services when they were disguised as medical service fees. According to court records, Aetna’s agreement with the Plan allowed it to outsource the work, but at its own expense; the Plan does not permit these administrative services fees to be passed along to participants.
Case info: Case info: Sandra M. Peters v. Aetna Inc., et al, Case No. 1:15-cv-00109-MR; US District Court, Western District Of North Carolina, Asheville Division; filed 06/05/2023
Among the relevant issues decided, whether Optum is a “provider” of the chiropractic and physical therapy services. The AMA, which is the is the author and copyright holder of CPT, took the position that network providers are the actual health care providers allowed to use CPT codes to bill, not companies such as Optum that contracted with Aetna to provide chiropractic and physical therapy services to the Aetna plan’s participants. The court agreed.
According to the court, “If [Optum] is a “provider” that simply subcontracts for the services and charges a fee for serving as the “general contractor,” then its arrangement is consistent with the Plan. On the other hand, if Aetna has simply contracted with Optum for Optum to provide some administrative services that Aetna had agreed to perform in its contract with the Plan,
“then the Aetna/Optum arrangement allows for charging a fee greater than allowed by the plan contract, and further serves to hide that excess fee from the Plan and its members by misidentifying it as part of a claim for services.”
Ultimately, the court held the following:
- “Plaintiff continues to have Article III standing to assert claims for disgorgement, surcharge, and (at least some forms of) declaratory and injunctive relief, both as an individual participant and on behalf of her Plan, without proof of a financial loss. As the Plaintiff has standing without proof of a financial loss to assert disgorgement/surcharge claims, both as an individual member and on behalf of her Plan, she also has standing to serve as a class representative on behalf of other individual members and self-insured plans who allege that Aetna likewise bypassed its obligation to pay Optum’s administrative fees with respect to their claims.”
- “A “Network Provider,”…is the “health care provider” that “has contracted to furnish services or supplies for this plan” and “is, with Aetna’s consent, included in the directory as a network provider.”
- “Optum’s renewed request to be dismissed from this action is therefore denied.”
- “The Court will certify this matter as a class action pursuant to Rule 23, with two classes of individuals, the Plan Claim Class and the Member Claim Class.
- Plan Claim Class: All participants or beneficiaries of self-insured ERISA health insurance plans administered by Aetna for which plan responsibility for a claim was assessed using an agreed rate between Optum and Aetna that exceeded the provider’s contracted rate with Optum for the treatment provided.
- Member Claim Class: All participants or beneficiaries of ERISA health insurance plans insured or administered by Aetna for whom coinsurance responsibility for a claim was assessed using an agreed rate between Optum and Aetna that exceeded the provider’s contracted rate with Optum for the treatment provided.”
As more and more of these cases make their way through the courts, self-insured health plan administrators charged with properly monitoring and safeguarding plan assets should do so, independent of their TPA’s own reporting. Additionally, as a result of this and other cases, including the Supreme Court’s decision to deny the Aetna/Optum’s challenge of the recent Fourth Circuit Court decision, these same self-insured health plan administrators, should seek return of Billions in plan assets.

We recently reviewed a BUCA ASO Agreement and wondered why a Plan Sponsor would ever sign it. The Agreement was a Contract of Adhesion, favoring the carrier at the expense of the Plan Sponsor. It was crafted to hobble any efforts at accountability. This article by Mark brings to light just one of those episodes where we find evidence of what can happen when these Agreements are in place. In this case it took a little ole plan member to question her EOB. Similar Blog Posting (There are hundreds like this on our blog) – Weslaco ISD vs Aetna

