By Russell Pekala
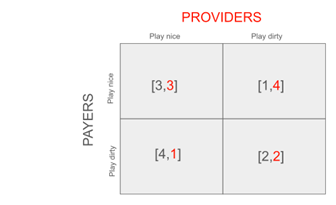
Setup: Providers (red) make a choice “Play nice” or “Play dirty” represented by the left and right columns and receive RED payouts. Payers make the same choice represented by the top and bottom rows and receive BLACK payouts
This is modeling out how a provider interacts with a payer in a *single* claim-generating situation.
Each has the choice of “Playing nice” with each other or “playing dirty” with each other.
Providers play nice by only recommending necessary treatment and cost/quality balanced referrals.
Payers play nice by paying claims quickly and completely and not requiring the provider to submit burdensome documentation.
If both the provider and the payer play nice, they will both pay/be paid a fair amount and spend nothing on legal or claim review.
If the payer plays nice but the provider plays dirty, the provider will be able to sneak in some subtle upcoding and improve their payout.
If the provider plays nice and the payer plays dirty, the payer will be able to justify delaying paying claims due to insufficient documentation.
If both play dirty, they will achieve a fair outcome but both spend a lot on legal and claim review.
Analysis: there is only one Nash equilibrium for this game, and it’s that the two parties end up both playing dirty.
Assuming the other side plays dirty, the other party would get a better payout playing dirty than playing nice.
It’s surprising but completely logical given the constraints and incentives of the game that the outcome achieved has the least total utility (total = 4) of the 4 possible outcomes.
This is why it’s called a dilemma after all!
It probably explains a little bit of intuition for why healthcare sucks.
Game Theory – Health Plans by Russel Pekala