Month: April 2009
Medicare Changes to Physician Compensation – The Impact on PPO Networks
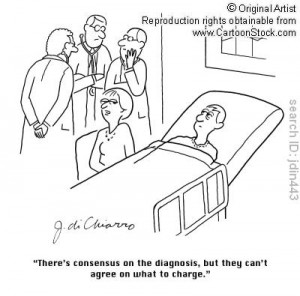
As I’ve been reporting for several months, Congressional Democrats and the President are working hard to increase reimbursement for cognitive services by up to 10%.
This would go a long way towards fixing what is perceived to be a core problem with US health care – overly generous compensation for procedures (surgery, imaging, etc) leads to over-utilization of those procedures, while under-reimbursement for office visits and other ‘primary care’ services results in a shortage of physicians willing to do primary care.
This morning’s New York Times features a headline story about the conflict in Washington, noting that the Obama Administration is very concerned about the shortage of primary care docs. The solution being discussed in DC is to get more applications into med schools.
Wrong answer.
The ‘right’ answer is staring us in the face – there are too many specialists, physicians who have already graduated from medical school and have lots of experience and training. It would be far easier, faster, and cheaper to re-train these physicians to take on more primary care responsibilities, albeit primary care with an orientation towards their specialty. Would this be difficult, and expensive, and meet with strong resistance from those docs?
Absolutely. But on balance it would be much easier, and faster, than waiting at least eight years for the supply of primary care docs to begin to meet anticipated demand.
Compensating docs more for primary care would potentially have another effect; it might reduce the volume of procedures performed, as specialists would also benefit from the higher compensation for evaluation and management services. I wouldn’t bet too much on this, as docs – like the rest of us – won’t change dramatically overnight. That said, increasing compensation for primary care service codes (the 99xxx CPTs) would help take a bit of the sting out of reduced reimbursement for surgery etc.
What does this mean for you?
A lot.
Most network contracts are based on Medicare’s RBRVS; if the Feds change, your provider compensation will too. Think about the potential impact, and think deeply. The trickle-down will likely cause specialists to seek higher network reimbursement for two reasons – first the base from which their reimbursement (RBRVS) has declined, and second, they’ll want to make up their lost revenue from Medicare by increasing reimbursement from private payers.
Texas’s Silent PPO Legislation
As the biennial Texas legislative session nears its end, it looks like the legislature may pass a bill that would have a dramatic effect on workers comp PPO networks.
According to WorkCompCentral (subscription required):
“HB 223 would regulate “discount brokers” that are engaged in (for money or other consideration) “disclosing or transferring a contracted discounted fee of physician or health care provider.” hb223
A broker could not transfer a physician’s or health care provider’s contracted discounted fee or any other contractual
obligation unless the transfer is authorized by a contractual agreement that complies with the provisions of the bill.
Those provisions include notifying each physician and provider of “the identity of the payers and discount brokers authorized to access a contracted discounted fee of the physician or provider.”
The notice must be provided at least every 45 days through “electronic mail, after provision by the affected physician or health care provider of a current electronic mail address” and posting of a list on a secure Internet website.”
Now that’s a huge change, one that would effectively stop much of the rental network business cold. The dirty secret of the work comp PPO business (well, one of the dirty secrets) is that networks don’t have direct contracts with providers in all states – every ‘national’ PPO uses another network’s contracts in at least a few jurisdictions.
Docs sign contracts in return for direction – they are trading a discount for the promise of more volume. Yet few networks actually drive any significant volume to the vast majority of their contracted physicians.
We’ve been seeing a rapid rise in the volume of litigation from providers contesting reduced reimbursement due to PPO contracts, with three payer clients reporting a significant upsurge in the last twelve months.
What does this mean for yuo?
Find a better, and more sustainable, way to reduce medical expense. The days of cutting costs by slashing provider reimbursement on the basis of some flimsy network contract are rapidly ending.
Editor’s Note: This was written by Joe Paduda
8,000 Life School District Seeks Insurance Bids
The Brownsville Independent School District is seeking competitive proposals for group health insurance – Specifications will be posted soon on: http://www.bisd.us/PURCHASING/bids_for_vendors.htm
Student Athletic Insurance for Texas School Districts
To the best of our knowledge, 100% of Texas school districts self-fund their group medical plans (TRS ActiveCare is a self-funded plan), yet 100% of Texas schools fully-insure their athletic insurance. We are wondering why. If districts save money through self-funding their medical plans, why cant they save money on student accident plans as well?
Basic student athletic insurance offers limited benefits. In addition to this basic cover, many districts purchase catastrophic cover starting at $25,000. It seems to us that it makes perfect economic sense to self-insure the limited benefits portion of the program and purchase stop-loss cover with a $25,000 retention. We have identified several carriers that will offer specific stop loss for student accident plans.
Districts can partner with area medical providers for the best cover at the lowest cost. After all, medical providers in the community are school district taxpayers too. They would support such a partnership.
One possibility to consider would be to fund an athletic insurance program through a captive with more than one school district participating through an interlocal agreement. Participating districts would then be able to participate in underwriting profits and maintain control of plan benefits and costs. An interlocal agreement would preclude districts from bidding out their student accident insurance every year.
$20,000 Bonus Offered By Major Health Carrier
An agent solicitation from a major health insurance carrier, sent out this week to agents throughout the United States, announces a $20,000 cash bonus to those agents who sell 20 group health insurance cases between April 1, 2009 and December 31, 2009. And, if the agent sells only 10 groups, the bonus is $10,000.
This is a powerful incentive to place business with this carrier, over another carrier wherein little or no bonus is offered. A broker, supposedly representing the client with whom he works for, may not disclose this arrangement. A conflict of interest would be apparent it would seem.
Acorn will surely get wind of this and organize a bus tour to homes of participating agents and brokers.
Carrier Provides PPO Specific Rates
Socialized Medicine Slated for Summer Vote
Congress began “debate” yesterday on health care. Pundits predict a Bill will be crafted by no later than June 1 upon which Congress will act. We predict passage of a sweeping national health care scheme that will bring this country firmly into an expanded welfare state.
Twitter – New Business Model for Carriers?
United HealthCare Opens 55,000′ Facility in Harlingen, Texas
The “Healthy Texas” Bill Passes Senate
TEXAS: The new “Healthy Texas” proposal targeting uninsured small businesses was passed in the Senate last week. The bill would allow a special insurance product to be offered to previously uninsured small businesses with at least 30 percent of its eligible employees receiving annual wages of less than 300 percent of the federal poverty level. The bill would require a 60 percent participation rate, and insurers would be responsible for all payments up to an annual threshold of $5,000 per individual. Once that threshold is met, the Healthy Texas Program would cover 80 percent of claims, up to $75,000, through a reinsurance fund for that individual.
Editor’s Note: This is an excerpt from an Aetna News Release to Agents & Brokers received today via email.
Susan Boyle
Are Insurance Consultants Biased?
In Texas, those in the insurance industry are a dysfunctional, yet close knit community wherein what one does in North Texas is common knowledge in South Texas and vice versa. Everyone knows everybody, and thus it becomes fairly easy to ascertain outcomes with various insurance consultants who work on behalf of their clients.
For example, one well known Dallas consultant, who specializes in assisting political subdivisions, made a video taped presentation to a county Commissioner’s Court wherein he stated that after an exhaustive and thourough review of area PPO network pricing, that “XXXX XXXXX” (insurance company) has the best PPO discounts by a minimum of 20%, and if you go with XXXX XXXXX you will save 20% off your claims next year.” This public statement put this consultant in a corner on subsequent assignments – he had no other option other than to recommend XXXX XXXXX on every analysis he did. In his next two assignments, as all of us predicted in advance, he moved the employer to XXXX XXXXX even though in both instances his methodology was flawed (we reviewed both cases after the fact and found the decision to move as problematic).
A well known (to us in the industry) and unknown (to uninformed employers) practice employed by some insurance consultants include dual compensation schemes – we will go into that in a later posting.(http://www.workforce.com/section/00/article/24/45/82.html)
An employer who is considering the services of a fee based insurance consultant, should ask for a listing of recent recommendations made to clients. A pattern may appear.
Many insurance consultants are biased. Analysis can be skewed honestly (with a dishonest intent). Numbers can tell any story one wants to tell. Employers can defend themselves by implementing certain defenses for effective and honest outcomes.
wall-street-journal-insurance-consultants
We have obtained a legal opinion (availble upon request) that Texas requires licensure to act as a fee-based insurance consultant. Two licenses are required: Life & Health Counselor License and Risk Manager License. Texas Department of Insurance lists of licensed insurance consultants can be found on the TDI website.
Could You Just Make a Decision? Please?
The following was written by Joe Paduda, 4-9-09 in Managed Care Matters:
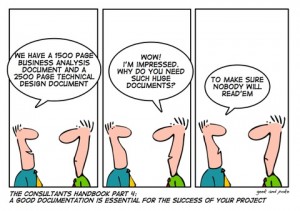
“TPAs and employers and insurance companies send out requests for proposal to each other, to managed care firms, specialty providers, voc companies, IT providers, law firms. All have been on the receiving end of a voluminous, detailed, structured and rigorous RFP – so big that it clogs their virtual and/or physicial mailbox.
The erstwhile vendor is initially happy. Hey, we made the cut, were on the list, we “get” to respond. We have an opportunity.
Then the work starts. Even if the vendor is big, and has staff to help write the responses, and even if it has a ready-made library of canned responses, it is still a lot of work. We arent talking a couple of hours here and there by a junior staff writer – every question has to be reviewed and assigned, then the answer checked for accuracy, grammer, and consistency with other answers. Then someone has to find all the reports and IT flow documents and disaster recovery plans and professional certifications and insurance coverage documents and CVs and make sure they have the right appendix numbers and are in the right format. Then it has to be collated, checked one more time, signed by an executive, and shipped out. All on the prospect’s schedule.
And that’s if it’s a big vendor; if it a small company, the folks who are doing this work are also the folks who are supposed to be doing the “real ” work – handling the tasks that actually deliver value to customers and owners alike.
The point is there is a lot of work involved, and most of the vendors who are doing the work are not going to get anything out of it – at least in terms of revenue. No, they’re going to have to savor the joys of a job well done, even if not done well enough to actually win the business.
I know, the “customer” has also put a lot of work into the process – no argument there. Just understanding what it is you want, what restrictions exist, what the timeline should be and who should be involved in the process from initial specs to final decision means meetings on top of meetings.
But just for a minute think about it from the vendor’s perspective. The erstwhile vendors want to deliver for your company, they think they can do a better job of anyone else, yet they’re forced to only answer what they’re asked, not allowed to demonstrate their abilities and insights and expertise and knowledge. Yes, they may be able to – in response to the “is there anything else we should know, or other ideas you have.” But the responses to these questions don’t fit the scoring methodology. Even if they are creative and innovative and fresh, and look promising, it’s tough for them to see the light of day in the typical RFP process.
Now comes the waiting, and the waiting, and the waiting.”
Editor’s Note: We sent this to an insurance consultant in Illinois. His comments: “Exactly…..which is why I rarely respond to public bid inquiries, and as a carrier (his previous employer) I did not either….also, when it comes right down to it….no one reads all the crap……they put you on a spreadsheet and then read later (if at all)…..I quote first with trusted vendors and then do the questions that really matter….when is the last time you had to worry about someone’s disaster recovery plan and whether or not it would work?”
We also rarely respond to RFP’s for the reasons stated by our friend in Illinois. Last year we bid on four jobs, along with the usual crowd of interested consultants. On one case, out of five respondents, our firm was ranked dead last. No interviews or follow up questions to the RFP were asked. Then, on another case, we responded to, we were competing with the same four consultants – the RFP included an interview process of all the respondents – we were ranked number one and obtained the business.
The Costs & Coverage Impacts Of A National Health Plan
The Lewin Group, a consulting firm, outlines their analysis of the impact of a National Health Insurance Plan in this report – http://www.lewin.com/content/publications/LewinCostandCoverageImpactsofPublicPlan-Alternative%20DesignOptions.pdf.
Hospital Billing Errors are Common
Why Your Hospital Costs Are Going Up
There’s little doubt hospital reimbursement methodology is going to change dramatically over the next few years.
We’re going to see a shift from fee for service to global episodic reimbursement, a shift that has already begun. I’ll get into that next week, but for now, there’s increasing evidence that private payers’ hospital costs are rising in large part due to several recent changes in reimbursement policies.
Over the last year, there have been three major changes in hospital reimbursement: the implementation of MS-DRGs (increase in the number of DRGs to better account for patient severity); a 4.8% cut in Medicare hospital reimbursement spread over three years; and the decision by the Centers for Medicare and Medicaid Services (CMS) to stop paying for ‘never ever’ events – conditions that are egregious medical errors requiring medical treatment.
The net result of these changes has been a drop in governmental payments to hospitals, the decision by several major commercial payers to not pay for never-evers, and increased cost-shifting from hospitals to private payers.
The implementation of MS DRGs and the accompanying decrease in reimbursement looks to be the most significant of the changes, and is already having a dramatic impact on hospital behavior patterns. By adding more DRG codes, CMS is acknowledging there are different levels of patient acuity – that performing a quadruple bypass on an otherwise-healthy patient takes fewer resources than doing the same operation on an obese patient with diabetes and hypertension. While these different levels were somewhat factored in to the ‘old’ DRG methodology, the new MS-DRGs better tie actual costs to reimbursement. (for a more detailed discussion, see here)
CMS projected that these changes would reduce Medicare’s total reimbursement for cardiovascular surgery by about $620 million, while orthopedic surgeries are projected to see an increase in reimbursement of almost $600 million.
Orthopedic reimbursement is increasing because there are now more MS DRGs for orthopedic surgery, and the additional DRGs will likely mean hospitals will be able to get paid more in 2009 and beyond than they were last year.
Hospitals are going to work very hard to get more orthopedic patients in their ORs, and they are going to carefully examine these patients to make sure they uncover every complication and comorbidity – because a ‘sicker’ patient equals higher reimbursement.
Editor’s Note: This is an excerpt sent to us by email this morning. We do not know the author or what publication this appeared in.
Legislative Update
This is an excellent synopsis of health care legislative matters published yesterday from Assurant