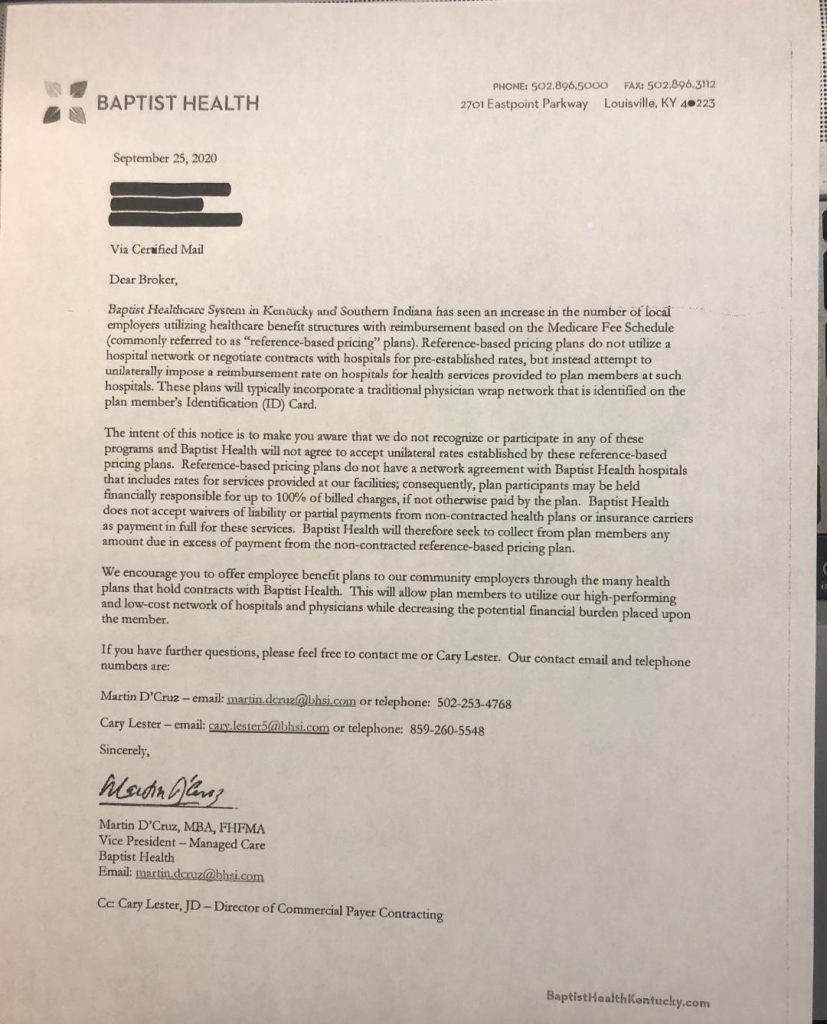
“The intent of this notice is to make you aware that we don’t recognize in any of these programs and Baptist Health will not agree to accept unilateral rates established by these reference based pricing plans…………..plan participants may be held financially responsible for up to 100% of billed charges”
By Bill Rusteberg
We’ve seen letters like this before. Designed to discourage plan sponsors from adopting transparent, fair and reasonable health care provider reimbursement strategies, we have seen an opposite effect.
Our first experience with this was back in 2008 in Eagle Pass, Texas, a one hospital town. The largest employer there, the Eagle Pass ISD, started a Reference Based Pricing plan for their 2,000 plus employees.
The local hospital was not happy and wrote a letter to members of the district’s Board of Trustees similar to the one shown above. The reaction they received was not what they expected.
The EPISD Board of Trustees and EPISD administration reside in Maverick County, Texas whose culture is akin to the Wild West of days gone by. “Maverick” perfectly describes the culture there.
The district responded by advising plan members of a new and improved benefit plan. Waiving all patient responsibility and covering all travel related expenses for both member and significant other, the district directed members seeking hospital / surgical care to San Antonio, about a two hour drive east.
Guess what happened after that?
The Eagle Pass ISD to this day remains on a Reference Based Pricing plan with easy access to their local hospital.
NOTE: The letter shown above was provided by Dan Meylan – Payer Compass

FROM A RISKMANAGERS.US CLIENT
A letter like this is pretty disingenuous. It’s a threat, pure and simple. They say the RBP’s unilaterally decide what a patient has to pay. Who says the Baptist Hospital has any more right to say what the customer is supposed to pay than the customer? Isn’t this still America where I have to agree to the charge? If they don’t list their price ahead of time, they have absolutely no right to claim the patient and/or plan has to pay the balance. That’s just utter bullshit, both ethically and legally.
In Texas, providers can’t send “disputed” bill information to a credit bureau anymore. All the patient and/or payer has to do is sit on the bills, ignore the calls, and go about their merry way. A company like AMPS definitely helps deflect the regular dunning. It gives a clueless and scared patient a partner and the reassurance to ignore the bills.
I had surgery in October 2017 – actually 3 different hospitalizations (thanks to a complication). I paid my copay, the plan paid what it was going to pay, and finally, after about 2 years, they gave up. No more calls; no more bills. And I didn’t even have to send a bill back with a big FU stamp on the front!!
EDITOR’S NOTE: As noted in the Eagle Pass case described in this blog entry, you can see here the reaction is almost always the same. People don’t like to be bullied, that’s human nature.

