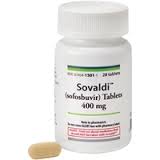
 The battle over the rising costs of drugs, fueled by Gilead’s Hepatitis C drug Sovaldi that costs $84,000 for a 12 week treatment regimen, intensified this week. Critics of the cost have taken to referring to the drug as the “1,000-a-day” pill.
The battle over the rising costs of drugs, fueled by Gilead’s Hepatitis C drug Sovaldi that costs $84,000 for a 12 week treatment regimen, intensified this week. Critics of the cost have taken to referring to the drug as the “1,000-a-day” pill.
By Nick Manetto
Earlier this week, the National Coalition on Health Care launched its Campaign for Sustainable Rx Pricing focused on the “unsustainable and abusive” prices of some drugs and that calls for finding “market-based solutions” to the issue. The Coalition, led by John Rother, the longtime AARP lobbyist, consists of many patient advocacy organizations as well as payers, unions and employers. Corporate members include Duke Energy, CVS Caremark, Premier and Verizon. Earlier in the year, state Medicaid programs and Medicaid Managed Care Organizations (MCOs) were among the first payers to express concerns given that many patients with the disease are Medicaid beneficiaries, and several state have acted to limit coverage of the drug.
On the other side of the issue is the biopharmaceutical industry, which argues that such novel treatments help improve lives and, in some cases, lead to lower healthcare costs over time. In the case of Sovaldi, advocates note that the treatment is far less costly – and less complicated – than a liver transplant. While expensive drugs are not new, Sovaldi is unique because of the more than 3 million U.S. patients who could benefit from the therapy and because of its superiority over existing treatment options: Following the treatment regimen, 90 percent of patients are cured of the disease.
Caught in the middle of the debate are patients and providers who typically want new and better treatments but also want them to be accessible and affordable. For proponents of Sovaldi and other novel therapies, demonstrating the economic benefits of the treatment over the long run may be helpful in pleading their case for coverage. At the same time, with the insurance market more fluid, payers have noted that there is no guarantee they will be the ones to realize the benefits should they cover a regimen only to have the now-cured patient move to another plan.
As one would expect, the issue has led some to compare the prices of the drug in the United States to costs in other nations that enact price controls. And earlier this year, leading Democratic members of the Energy & Commerce committee sent a letter to Gilead’s CEO asking questions about the pricing of the drug.

