 “It is outrageous that a TPA/audit firm, who uses their own client’s buying power, will turn around and sell them access to a contract that is worse than Cost Plus, and as a result increase their net fees!”
“It is outrageous that a TPA/audit firm, who uses their own client’s buying power, will turn around and sell them access to a contract that is worse than Cost Plus, and as a result increase their net fees!”
By Homer G. Farnsworth, M.D.
“If you move away from your managed care contract, you will save at least 40% above and beyond what you are paying now!” Such is the usual opening statement at the beginning of every sales call these days. The Cost Plus Health Insurance revolution continues to gain traction.
The key to Cost Plus is based upon paying medical providers fair and reasonable fees utilizing universal benchmarks that are defensible and can be quantified up front with predictable underwriting results. Bench marking off Medicare allowed reimbursement rates or cost-to-charge ratios as reported to CMS is the keystone to Cost Plus Insurance.
Direct contracting with interested providers is a natural extenstion of the scheme. Therein lies the rub – does a plan sponsor who enters into a direct contract negotiated by a third party, one who is stepping back into the murky world of managed care?
All depends who does the negotiation. If a plan sponsor empowers their TPA and audit firm to negotiate, the final result may be contract with ownership between the audit/TPA firm and the contracted provider. In that case the plan sponsor ends up as a third party beneficiary only, just like they were under their previous PPO plan.
Why would a TPA/audit firm negotiate away their revenue stream? The answer is they don’t. In fact, many times, in terms of work performed, they may earn more money negotiating direct contracts for their clueless clients with much less work involved. And they will continue to get paid for doing nothing..
Ironically, using the buying power of their own client, the TPA/audit firm negotiates a contract and then turns around and sells access to the benefits of the contract back to the client/s whose purchasing clout drove the negotiating effort in the first place.
The “direct” contract is usually touted to be the “equivalent of Medicare +35%”, or “a really good contract that is better than a typical PPO contract.” After review, it is apparent both statements are essentially correct since the two representations cited above are broad enough to emcompass any number of defensible arguments. A clueless plan sponsor, with an equally clueless insurance broker/consultant, is thus pacified and supportive. Hallelujah!
However, the contract includes many of the things a typical PPO contract has, including an annual escalater clause. Every 12 months the contract gets worse by at least 6%. And, although some of the reimbursement levels approximated 135% of Medicare, other expenses are segregated and added to bill, making the contracted rate for a particular claim as much as, or greater than a typical PPO reimbursement rate at the same hospital. And the contract is certainly more costly to the self-funded plan sponsor than a Cost Plus approach.
It would appear the TPA/audit firm has successfully “negotiated away” their fees. But, secretly they revel in their coup – they have succeeded in earning more money for less work, all at the expense of their own client.
Unfortunately, the plan sponsor is now captive. They do not own the contract. They have no ability to negotiate the contract upon renewal, nor is there any incentive for the TPA/audit firm to continue to seek better terms.
We have found that some TPA/audit firms charge a percentage of “savings” under these direct contracts as much as 10%. To charge a fee based on arbitrary charge master rates on a negotiated contract that precludes any balance billing issues or even lawsuits is outrageous in the view of some in the industry. Molly Mulebriar, insurance reporterette for the Waring Times, states “It is outrageous that a TPA/audit firm, who uses their own client’s buying power, will turn around and sell them access to a contract that is worse than Cost Plus, and as a result increase their net fees!”
A good example of professional fleecing could be illustrated by a hospital bill of $100,000. Under Cost Plus, the TPA/audit fees to process and defend the claim would be as much as $12,000 (fee based on 12% of gross billed charges). This fee includes line-by-line audit, balance bill defense, claim appeals, and potential lawsuits.
However, under a TPA/audit “direct” contract the net fee to be earned for doing essentially nothing could be approximately $7,500. In terms of work performed, the payout is far greater.
Other TPA/audits firms who we know to be active in the Cost Plus market, would charge approximately $3,750 (5% of allowed), or about half the fee a “direct” contract would cost a plan sponsor. Which is better, pay $7,500 fee to access a contract through which you pay a higher reimbursement rate, or pay $3,750 audit fee to pay lower reimbursement rate on a Cost Plus basis? Never before has paying more for more, or paying less for less taken on a whole new meaning, an oxymoron in reverse.
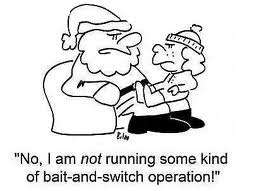
So the question becomes: “Did the TPA/audit firm bait their client into Cost Plus, only later to switch them back to a managed care contract they control?

