 Another vendor, touting a NEW strategy to reduce health care costs, enters the Reference Based Pricing arena. They, along with the rest of their competitors are 35 years late in identifying the concept. Back in the early 1980’s J Patrick Rooney (1927 – 2008) contended that authoritative research showed that Medicare plus 25 percent is the reasonable amount for hospitals to charge. Then, of course, there is J.P.Farley (www.jpfarley.com)who has actually been implementing Reference Based Pricing plans since the 1990’s……………………….
Another vendor, touting a NEW strategy to reduce health care costs, enters the Reference Based Pricing arena. They, along with the rest of their competitors are 35 years late in identifying the concept. Back in the early 1980’s J Patrick Rooney (1927 – 2008) contended that authoritative research showed that Medicare plus 25 percent is the reasonable amount for hospitals to charge. Then, of course, there is J.P.Farley (www.jpfarley.com)who has actually been implementing Reference Based Pricing plans since the 1990’s……………………….

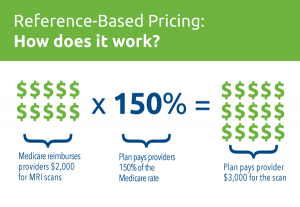
In recent years, a new tool has emerged in the industry to help control health benefit costs, both for health plans and for members: Reference-Based Pricing. Under reference-based pricing, plan sponsors agree to pay all providers a set price for the same services, based on reference benchmarks, often a percentage of Medicare or provider cost data.
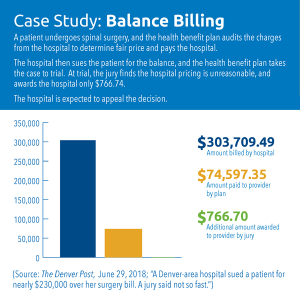
In instances where the provider charges more than the amount the plan is willing to pay, the provider may send a bill to the patient for the balance. This is called balance billing. Depending upon the specific details of the patient’s plan, CoreSource has teamed up with advocates who minimize disruption and provide resources to defend the member against balance billing.In the rare cases when providers have taken balance billing cases to court, advocates are there to assist and defend members.
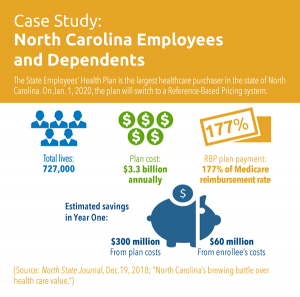
For a deeper look at how reference-based pricing could change the industry, our own Matt Brannigan and Lee Rufty examine the pros and cons of reference-based pricing, including the proposed plan by the state of North Carolina to switch the state employee’s health benefits plan to reference-based pricing in 2020.
With this move, the state is taking more control over what it will pay for its employees’ healthcare, shifting away from a top-down, network-style negotiation to a more bottom-up focus. Representing as many lives as it does, and paying out over $3 billion each year to providers, North Carolina is able to flip the script on negotiations. Instead of asking “what kind of a deal can you give us?” the state can simply say “here’s what we’re willing to pay, based on the Medicare reimbursement rate. Are you in or out?”
Reference-Based Pricing: a Welcome Disruption
 Naturally, for reference-based pricing to best succeed, it’s important for members and plan administrators to understand how these plans are different from traditional PPO models and how reference-based programs will support them.
Naturally, for reference-based pricing to best succeed, it’s important for members and plan administrators to understand how these plans are different from traditional PPO models and how reference-based programs will support them.
Depending on the health benefit plan design, members may now be balance billed for costs incurred above and beyond the fair market cost as determined by our models. Member education is key to alleviating any pain points that come from this change.
Reference-Based Pricing: Antidote to Rising Healthcare Costs
To learn more about reference-based pricing and how it can help your clients, contact us or call your CoreSource sales executive.

