“Pharmacists have long been concerned with pharmacy benefit managers operating as largely unregulated middlemen in the drug supply chain………………..”
Pharmacy Associations Urge Senate Judiciary Committee to Hold Hearing on PBMs
by NCPA | Apr 09, 2018
ALEXANDRIA, Va. (April 9, 2018) — The National Community Pharmacists Association and 46 state pharmacy groups sent a letter urging the U.S. Senate Judiciary Committee to hold a hearing on the problematic business practices of pharmacy benefit managers, the middlemen who administer prescription drug benefits for health plans.
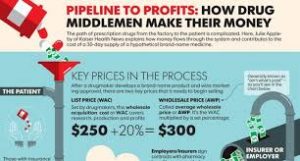
“Pharmacists have long been concerned with pharmacy benefit managers operating as largely unregulated middlemen in the drug supply chain,” the letter states. “While PBMs claim to keep drug costs low, we believe many PBM practices are anti-competitive and ultimately drive up health care costs for consumers and plan sponsors while reducing payments to pharmacies.”
The letter added, “Recently, two of the big three PBMs announced acquisition plans with large insurers (CVS Health to acquire Aetna Inc. for $69 billion; Cigna to acquire Express Scripts for $67 billion). If these acquisitions proceed, all three of the largest PBMs will be vertically integrated with an insurance company, since UnitedHealth Group Inc. currently owns OptumRx. The potential harm from such continued market concentration should be closely examined.”
The specific areas of concern the committee was asked to investigate are:
- The lack of oversight of PBMs at the federal and state level.
- One-sided business arrangements that disadvantage pharmacies in their contracts with PBMs.
- Spread pricing models that allow non-transparent PBMs to pocket the difference between what they reimburse pharmacies and what they charge health plan sponsors.
- Self-dealing, where PBM-affiliated pharmacies are reimbursed at higher rates than their pharmacy competitors.
- The inherent conflicts of interests of PBMs owning mail-order pharmacies that directly compete with community pharmacies.
- The high cost and lack of transparency associated with the brand-name drug manufacturer rebates PBMs
- The use of retroactive pharmacy direct and indirect remuneration fees that hurt pharmacy cash flow and operations, while also increasing costs to Medicare Part D beneficiaries and tax payers.
- The exclusion of community pharmacies from Part D preferred pharmacy networks.
###
The National Community Pharmacists Association represents the interests of America’s community pharmacists, including the owners of more than 22,000 independent community pharmacies. Together they represent an $80 billion health care marketplace and employ more than 250,000 individuals on a full- or part-time basis. To learn more, go to www.ncpanet.org, visit facebook.com/commpharmacy, or follow NCPA on Twitter @Commpharmacy.

