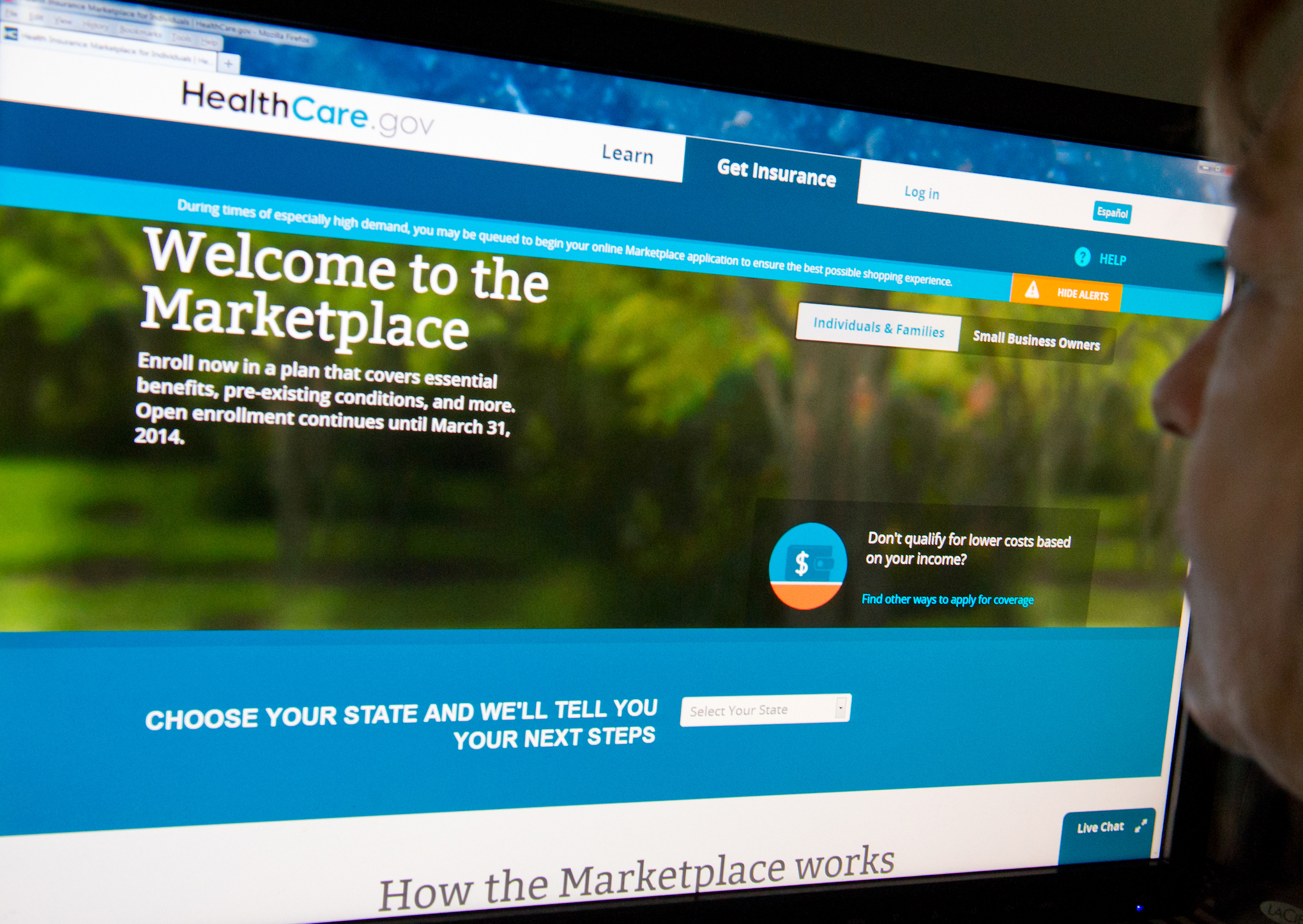
A loophole in Obamacare regulations has health plans worried that people who bought coverage on the federal marketplace could skip their December payment and insurers would have few tools available to recoup that missed premium.
“People can get a free month of health care,” says one insurance industry official, who flagged the issue and requested anonymity to speak openly about the problematic guidance. “If they knew about the rule, they functionally wouldn’t have to pay for their last month of coverage.”
A collision of Obamacare regulations

Senate Minority Leader Mitch McConnell (R-Ky.) stands next to a tower of all Obamacare regulations (Alex Wong / Getty Images)
Obamacare guarantees enrollees a three-month grace period if they fall behind on their premiums. Someone who stops paying in March, for example, has through May to make good. So if they don’t pay up in March but have a medical bill in May, they can get that bill covered by paying their back premiums. It’s only after May that they’re really uninsured.
And if someone misses their grace period entirely — doesn’t pay in March, or April or May — federal guidance published July 16 specifies that their coverage runs out on the “last day of the first month of the grace period.” In this hypothetical example, the person who never paid for March, April and May would still get coverage through March 31.
“IF THIS NOTION CAUGHT ON, IT COULD BECOME SOMETHING ROUTINELY ABUSED”
That same federal guidance has other important instructions for how to handle subscribers’ payments for 2015. It says that if an Obamacare shopper goes online and re-enrolls in a new insurance plan, any payments towards that new, 2015 plan cannot be applied to outstanding debt on the old, 2014 plan.
This, insurers worry, is what could make December a bit of a no-man’s land for insurers looking to get paid. Somebody could theoretically refuse to pay up in December 2014 and then rejoin their plan — or buy a new one — in January or February of 2015. The health plan they had in December can’t terminate their coverage or use their new premiums to to cover the outstanding debt.
“WE CAN’T DO ANYTHING IF YOU HAVE A NEW, 2015 POLICY”
“What happens is you have all of December and January and February to pay that December 2014 premium,” says the insurance source, describing the situation. “If you still haven’t paid by February, what we would typically do is terminate your policy. But we can’t do anything if you have a new, 2015 policy.”
Insurers could send a collection agency after someone who never paid their December premium. But they argue that using collections is draconian and inefficient, particularly against the low-income population the exchanges often serve. Insurers see the federal government as essentially stripping them of their normal tools for ensuring that members pay premiums: canceling the plans of those who are delinquent and, when members do pay, applying that premium to their outstanding debt.
Aaron Albright, a spokesman for the Centers for Medicare and Medicaid Services, said that consumers are still required to pay their December premium, just as they are any other month when they receive coverage.
“Grace periods are important to ensure that consumers aren’t dropped from coverage, especially for those experiencing economic challenges,” he said in an emailed statement. “However, consumers are still responsible for paying their outstanding premium to their insurance company for the period they were covered.”
Health plans suggested fix: Apply new premiums to old debt
(Karen Blier / AFP)
Health insurers want to see Health and Human Services change their regulations to allow them to apply any new payment to outstanding debt. Under this scenario, insurers would be able to use 2015 premium dollars to cover months left unpaid in 2014.
Insurance plans also say this would solve a logistical headache, too: the computer systems they currently use are set up to apply all new payments to whatever outstanding debts a consumer has. In order to make the current payment system work, they might have to set up two separate accounts for the same subscriber.
“There’s a significant operational issue because the current billing systems were set up to apply someone’s most recent payment to their oldest outstanding balance,” a second insurance industry source says. “We have people working on that issue right now.”